Abstract
Background
Tourniquet use during total knee arthroplasty (TKA) improves visibility and reduces intraoperative blood loss. However, tourniquet use may also have a negative impact on early recovery of muscle strength and lower extremity function after TKA.
Questions/purposes
The purpose of this study was (1) to determine whether tourniquet use affects recovery of quadriceps strength (primary outcome) during the first 3 postoperative months; and (2) to examine the effects of tourniquet application on secondary outcomes: voluntary quadriceps activation, hamstring strength, unilateral limb balance as well as the effect on operative time and blood loss.
Methods
Twenty-eight patients (mean age 62 ± 6 years; 16 men) undergoing same-day bilateral TKA (56 lower extremities) were enrolled in a prospective, randomized study. Subjects were randomized to receive a tourniquet-assisted knee arthroplasty on one lower extremity while the contralateral limb underwent knee arthroplasty without extended tourniquet use. In the former group, the tourniquet was inflated just before the incision was made and released after cementation; in the latter group, a tourniquet was not used (10 of 28 [36%]) or inflated only during component cementation (18 of 28 [64%]). The choice of no tourniquet or use just during cementation was based on surgeon choice, because some surgeons felt a tourniquet during cementation was necessary to achieve a dry surgical field to maximize cement fixation. A median parapatellar approach and the identical posterior-stabilized TKA design were used by all four fellowship-trained knee surgeons involved. Isometric quadriceps strength, hamstring strength, voluntary quadriceps activation, and unilateral balance were assessed preoperatively, 3 weeks, and 3 months after bilateral knee arthroplasty. Other factors, including pain, range of motion, and lower extremity girth, were assessed for descriptive purposes at each of these time points as well as on the second postoperative day.
Results
Quadriceps strength was slightly lower in the tourniquet group compared with the no-tourniquet group (group difference = 11.27 Nm [95% confidence interval {CI}, 2.33–20.20]; p = 0.01), and these differences persisted at 3 months after surgery (group difference = 9.48 Nm [95% CI, 0.43–18.54]; p = 0.03). Hamstring strength did not differ between groups at any time point nor did measures of quadriceps voluntary activation or measures of unilateral balance ability. There was less estimated intraoperative blood loss in the tourniquet group (84 ± 26 mL) than in the no-tourniquet group (156 ± 63 mL) (group difference = −74 mL [95% CI, −100 to −49]; p < 0.001). However, there was no difference in total blood loss between the groups (group difference = −136 mL [95% CI, −318 to 45]; p = 0.13).
Conclusions
Patients who underwent TKA using a tourniquet had diminished quadriceps strength during the first 3 months after TKA, the clinical significance of which is unclear. Future studies may be warranted to examine the effects of tourniquet use on long-term strength and functional outcomes.
Level of Evidence
Level I, therapeutic study.
Similar content being viewed by others
Introduction
Application of a tourniquet during TKA has been frequently used to improve visualization of the operative field, decrease intraoperative blood loss [11, 14, 17, 22, 27, 60, 65], and improve the quality of cementation by providing a relatively bloodless operative field [21]. A 2010 analysis of current practice patterns of members of the American Association of Hip and Knee Surgeons found 95% of patients without vascular disease who underwent TKA had their procedures performed under tourniquet control [7].
Some reports have found numerous disadvantages associated with tourniquet use, including reduced early knee flexion [11, 14, 60, 62, 65], increased perioperative pain [11, 14, 27, 56, 57], increased postoperative limb swelling [11, 21, 47], more frequent wound complications [9, 12, 40, 41], an increase in cardiac and cerebral microemboli [16, 20, 42–44, 55], an increased incidence of deep venous thrombosis [8, 57, 65], an increased risk of arterial thrombosis in subjects with preoperative vascular disease [22, 26, 48], a risk of peripheral nerve injury [29, 39], and skin irritation from tourniquet application [13].
Limited research has been conducted to evaluate the effects of tourniquet use on postoperative rehabilitation and early functional strength recovery after TKA. The purpose of the current randomized controlled trial is to determine whether tourniquet use during TKA affects (1) the recovery of quadriceps strength; and (2) other factors including voluntary quadriceps activation, hamstring strength, and unilateral limb balance.
Patients and Methods
This prospective randomized controlled study was conducted by a team of researchers at Colorado Joint Replacement and the Department of Physical Medicine and Rehabilitation at the University of Colorado School of Medicine and approved by the institutional review board and ethics committee at Porter Adventist Hospital. The Colorado Multiple Institutional Review Board, which oversees human subjects’ research at the University of Colorado Anschutz Medical Campus, also reviewed the study protocol and ceded to the institutional review board at Porter Adventist Hospital. Patients undergoing same-day bilateral TKA were recruited and tested between October 2012 and August 2014.
Patients were eligible for inclusion if they elected to undergo simultaneous bilateral TKA for knee osteoarthritis and were deemed appropriate surgical candidates for such a procedure. Exclusions included medical risk factors that precluded a bilateral TKA surgical operation and unstable orthopaedic or neuromuscular conditions (including hip pain) that could differentially influence lower extremity recovery and performance after TKA. Potential between-group confounders such as baseline demographics or other systemic factors (such as medical comorbidities) were accounted for by the within-subject design, wherein each patient’s limbs were randomized to receive one of two procedures: (1) TKA performed with use of a tourniquet; or (2) TKA during which a tourniquet was not used or was inflated only for component cementation (no-tourniquet group).
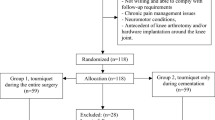
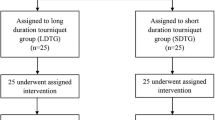
Fifty patients were screened for inclusion in this randomized controlled trial. Thirty-two patients (64 knees) agreed to participate, whereas 18 refused to participate in the study. During the period of this analysis, 118 same-day bilateral knee TKAs were performed at our center. Two patients participated in preoperative strength and functional assessments but subsequently underwent unilateral TKA and were withdrawn from the study. One additional patient required a total synovectomy as a result of proliferative synovitis (unanticipated before surgery) during TKA of the tourniquet limb. Because of the strong potential for between-limb surgical differences to confound postoperative comparisons in strength and functional outcomes, this patient was withdrawn before followup evaluation. Finally, one participant did not return phone calls or emails after surgery and was lost to followup. All other patients (N = 28; 16 male, 12 female) were included in the analysis. The average age of the study population was 62 ± 6 years, and the average body mass index was 29 ± 4 kg/m2.
Randomization was computer-generated, in permuted blocks of two or four, by a research assistant (KS) who was not involved in patient care and did not perform any of the study assessments. Surgeons were informed of limb assignment for each patient 24 hours before the operative procedure. During the operation, patients underwent the initial TKA on the right lower extremity, regardless of group assignment, so that a potential order effect could be accounted for in the analysis. Fourteen patients had the right lower extremity randomized to the no-tourniquet group (left lower extremity randomized to undergo the tourniquet procedure), whereas the other 14 patients had the left lower extremity randomized to the no-tourniquet group. Leg dominance was not assessed. Patients, physical therapists, nurses, and research assistants involved in study assessments were blinded to group assignment.
All TKAs were performed by surgeons of Colorado Joint Replacement according to a standard protocol. Spinal anesthesia plus a single local anesthetic injection femoral nerve block for each limb was used for all patients. Appropriate perioperative parenteral antibiotics were administered in all patients for infection prophylaxis. For limbs assigned to the tourniquet group, a pneumatic tourniquet placed high on the thigh was inflated to 250 mmHg before the skin incision. The tourniquet was released on completion of cementation of femoral, tibial, and patellar components. For limbs in the no-tourniquet group, a tourniquet was not used (10 of 28 [36%]) or inflated only during component cementation because some participating surgeons felt a tourniquet was necessary to minimize blood at the bone-cement interface and maximize fixation (18 of 28 [64%]). All TKAs, regardless of group assignment, were performed using a medial parapatellar approach and a gap balancing technique with substitution of the posterior cruciate ligament. The same implant design was implanted into both knees of each individual subject. Hemostasis was achieved by electrocautery. Before wound closure, all knees received an intraarticular (synovium, periosteum, posterior capsule, and arthrotomy site) injection of a cocktail containing ropivicaine, epinephrine, clonidine, and ketorolac to enhance postoperative analgesia. Intraarticular drains were used in all TKAs and were removed on the morning of the first postoperative day. Operative and tourniquet times were recorded for all procedures. Intraoperative blood loss was estimated from suction drainage volume and lap sponges. Postoperative blood loss was recorded by the inpatient nursing staff from that collected in the suction drain reservoirs.
Anticoagulation regimens, postoperative pain management, and other systemically delivered therapies, which were deemed unlikely to have a differential effect on right versus left knees, were administered according to the preferences of individual surgeons. Inpatient physiotherapy was delivered according to hospital protocols, and all patients participated in a similar outpatient physiotherapy program three times weekly for a minimum of six weeks.
Study assessments for primary and secondary outcomes (except for operative measures) were performed at the University of Colorado Anschutz Medical Campus preoperatively and at 3 weeks and 3 months after the bilateral TKAs. Isometric torque for quadriceps and hamstring muscles was also measured during the hospital stay using different instrumentation. Assessments of other outcomes (pain, swelling, range of motion) were performed at these time points as well as during the hospital stay on the second postoperative day.
For the main study endpoints (preoperative, 3 weeks, 3 months), isometric quadriceps muscle torque (primary outcome) and hamstring torque (secondary outcome) were measured during a maximum voluntary isometric contraction (MVIC) using a HUMAC NORM (CSMi, Stoughton, MA, USA) electromechanical dynamometer. Data were collected with a Biopac Data Acquisition System at a sampling frequency of 2000 Hz (Biodex Medical Systems, Inc, Shirley, NY, USA). Quadriceps and hamstring strength assessments were performed twice and the maximum voluntary torque value was recorded. If maximal torque differed by more than 5%, a third trial was performed. Quadriceps activation testing was performed using the doublet interpolation test, as previously described [5, 6, 32]. A value of 100% represents full voluntary muscle activation, and anything less than 100% represents a deficit in muscle activation (incomplete motor unit recruitment or decreased motor unit discharge rates). The hamstrings were not tested for voluntary activation. The unilateral balance test, a common test of static balance [30], was chosen as a surrogate measure of unilateral knee function.
To measure strength in the inpatient setting, a force transducer device (Lebow Products, Troy, MI, USA), which had been validated in pilot testing against an electromechanical dynamometer, was used to measure the force of MVIC of the hamstring and quadriceps muscles. This device was chosen to maximize the accuracy of strength assessments in the early postoperative period, when electromechanical dynamometry was not accessible. The methodology of this testing is further described in an electronic appendix (Appendix 1 [Supplemental materials are available with the online version of CORR®.]).
Other measures that were assessed for descriptive purposes included an assessment of knee active range of motion (AROM), measured in the supine position using a long-arm goniometer as previously described [38]. When measuring active knee extension, the heel was placed on a 4-inch block and the participant was instructed to actively extend the knee. Negative values of extension represented hyperextension. For active knee flexion, the participant was instructed to actively flex the knee as far as possible keeping the heel on the supporting surface. Calf girth (20 cm proximal to the medial malleolus), knee girth (suprapatellar), and thigh girth (10 cm proximal to the superior border of the patella) were recorded to assess lower extremity edema. Finally, pain was measured using an 11-point verbal numeric pain rating scale. Patients were asked to rate the pain in each knee on a scale of 0 to 10 with 0 representing no pain and 10 representing the worst pain imaginable.
To our knowledge, there is no agreed-upon minimal clinically important difference (MCID) in quadriceps strength outcomes for patients undergoing TKA. Therefore, we chose to base our estimate of sample size on our desire to detect a small to medium effect (Cohen’s d < 0.4) on quadriceps strength at our primary endpoint (3 weeks after surgery). Based on our previous work [51, 53], we assumed a standard deviation in quadriceps strength of 29.8 Nm at 3 weeks after surgery and estimated that 25 patients (50 knees) would be required to achieve 90% power to detect a small to medium effect (approximately 12 Nm) at this time point. Sample size estimates were performed using Statistical Analysis Software (SAS Institute Inc, Cary, NC, USA). To recruit a sample of 50 knees through 3 weeks after surgery, a total of 32 patients were enrolled with 28 patients (56 knees) completing testing at 3 weeks and 26 patients (52 knees) completing testing at 3 months.
Our study was underpowered to assess complications, which were indeed uncommon and summarized as follows: one non-fatal pulmonary embolism (origin unknown), one asymptomatic deep vein thrombosis in a limb assigned to the no-tourniquet group, and one traumatic wound dehiscence for a limb assigned to the tourniquet group that was managed surgically and that precluded 3-month strength testing.
The primary outcome measure, a difference in isometric quadriceps muscle torque between tourniquet and no-tourniquet groups at 3 weeks postoperatively, was evaluated using maximum likelihood estimation of a multivariate, repeated-measures model. This analysis was chosen to allow us to control for the order of surgery. The model computed the difference between limbs at each time point, providing a paired comparison that is analogous to a repeated-measures analysis of variance. This method also avoids case-wise deletion of missing data with the maximum likelihood estimate calculated under the assumption that missing data are missing at random [61]. Group differences in operative time, tourniquet time, and blood loss were evaluated with paired t-tests. SAS Version 9.3 was used for all statistical analyses. A two-sided alpha level of 0.05 was designated for statistical significance.
Results
Although no differences were found at baseline, by 3 weeks after TKA, quadriceps strength was lower in the tourniquet group compared with the no-tourniquet group (group difference = 11.27 Nm [95% confidence interval {CI}, 2.33–20.20]; p = 0.01; Table 1), and these differences persisted at 3 months after surgery (group difference = 9.48 Nm [95% CI, 0.43–18.54]; p = 0.03). On the second postoperative day, we found no differences in quadriceps strength. Hamstring strength did not differ between groups at any time point nor did measures of quadriceps voluntary activation or measures of unilateral balance ability (Fig. 1).
Group means for no-tourniquet (NoTQT) and tourniquet (TQT) limbs are displayed at each time point (mean ± SEM at each time point). Changes over time are shown for (A) maximum isometric quadriceps torque, (B) maximum isometric hamstring torque, (C) quadriceps voluntary activation, and (D) unilateral balance test. *Difference between NoTQT and TQT groups is significant at the p < 0.05 level. UBT = unilateral balance test.
There was less estimated intraoperative blood loss in the tourniquet group than in the no-tourniquet group (group difference = −74 mL [95% CI, −100 to −49]; p < 0.001; Table 2). However, group differences in total blood loss did not reach statistical significance (group difference = −136 mL [95% CI, −318 to 45]; p = 0.13). Operative time did not differ between limbs assigned to the tourniquet procedure (62 ± 11 minutes) and limbs assigned to the no-tourniquet procedure (65 ± 10 minutes). As expected, the average tourniquet time in the tourniquet group was greater than the no-tourniquet group (group difference = 42 minutes [95% CI, 37–47]; p < 0.001).
Descriptive statistics for other outcomes (pain, lower extremity girth, and AROM) are reported (Table 3). Visual inspection of group means suggests against a clinically meaningful difference between tourniquet and no-tourniquet approaches.
Discussion
A recent practice survey demonstrated a predominance of knee arthroplasties are performed using a tourniquet [7]. Advantages of tourniquet use include improved visualization, reduced intraoperative blood loss, and enhancement of cement fixation [11, 14, 17, 21, 22, 27, 45, 54]. Reported adverse effects of tourniquet use include reduced early knee flexion [11, 14, 60, 62, 65], increased perioperative pain [11, 14, 27, 56], postoperative limb swelling [11, 21, 47], wound complications [9, 12, 40, 41], and creation of cardiac and cerebral microemboli [16, 20, 42–44, 55]. Additionally, some have reported an increased incidence of deep venous thrombosis [8, 57, 65], arterial thrombosis in subjects with preoperative vascular disease [26, 48, 49], and peripheral nerve injury [28, 39]. This study was designed to determine if tourniquet use during TKA affected postoperative functional recovery, particularly the return of quadriceps strength, as well as secondary measures such as hamstring strength, quadriceps activation, unilateral balance, and the amount of perioperative blood loss. A bilateral TKA study model with both operative procedures performed at the same surgical setting was chosen to minimize between-group confounding variables. Each patient served as their own control; the rehabilitation program was identical and simultaneous for each TKA, and each TKA was equally affected by potential systemic adverse medical events.
Our results showed greater quadriceps strength when a tourniquet was not used, at both 3 weeks (approximately 14% greater) and 3 months (approximately 7% greater) after surgery. The authors hypothesize the reduction in quadriceps strength is multifactorial and likely related to muscle damage from tourniquet-induced ischemia or direct compressive injury. In those patients who experience increased pain from tourniquet use, the increased pain may result in some degree of quadriceps inhibition. Abdel-Salam and Eyres [1] assessed quadriceps strength in a comparative study of patients undergoing TKA performed with or without a tourniquet using the time required for the patient to perform a straight leg raise maneuver. Quicker ability to achieve this activity was observed in subjects in whom a tourniquet was not used. Ejaz et al. [14] studied a cohort of 70 patients undergoing TKA in whom only 35 were randomized to receive a tourniquet. Patients treated without a tourniquet demonstrated superior outcome in all Knee Injury and Osteoarthritis Outcome Score subscores and better early knee AROM out to 8 weeks postoperatively. Mittal et al. [33] in a similar comparative study found no differences in Oxford knee scores at 10 weeks after TKA.
To our knowledge, there is no agreed-upon clinically important difference in quadriceps strength for this population. Nevertheless, quadriceps weakness is a hallmark of TKA [4, 34, 52]. Although other measures of physical function typically recover over the first 3 postoperative months, quadriceps strength appears to take the better part of a year to recover to preoperative levels (and may fail to fully recover for many patients) [4, 34]. Early postoperative deficits in quadriceps strength may be particularly problematic because there is reason to believe that early strength loss, occurring primarily through deficits in voluntary muscle activation [36], may actually exacerbate long-term weakness [24]. In fact, there is a growing body of research focused on improving TKA rehabilitation specifically to limit early postoperative loss of quadriceps strength [31, 53]. Moreover, for patients undergoing TKA, quadriceps strength is one of the most robust predictors of long-term function in tasks such as chair-rise and stair-climbing ability [35, 64]. The strength differences we observed are comparable in effect size to what has been observed in studies of traditional versus minimally invasive (or quadriceps-sparing) TKA [23, 51]. Future research might consider combination approaches (eg, reduced tourniquet use in combination with quadriceps-sparing surgical techniques) to optimize strength recovery. Currently, the decision of whether to use a tourniquet should be influenced by many potential risks and benefits that must be individualized for each patient and also influenced by surgeon confidence that they can perform a TKA with the same precision without as with the use of a tourniquet.
Limitations of this report include that testing was continued to only 3 months postoperatively. The focus of this report, however, was to investigate the effects of a tourniquet on early TKA recovery. Second, the sample size may not be large enough to determine statistical significance for all variables tested such as quadriceps voluntary activation, unilateral limb balance, and blood loss. Such measures warrant inclusion in future research of tourniquet effects on postoperative recovery, and the effect sizes observed in this study could be used to inform sample size estimates for future studies, if examination of statistical significance in these outcomes is deemed clinically relevant. Previous work performed by the authors [51, 53] suggested that 25 patients (50 knees) would be required to achieve 90% power to detect a small to moderate effect of tourniquet use on quadriceps strength at 3 weeks postoperatively, the primary variable of this report. Because leg dominance was not formally assessed in this study, it is conceivable that—by chance—the tourniquet could have been applied to the nondominant leg a greater proportion of the time, thus confounding outcomes in favor of the no-tourniquet group. However, given that no group differences were observed at baseline in primary or secondary outcomes, we consider it likely that our randomization was successful in accounting for between-limb differences. Future work could consider incorporating assessments of leg dominance or other measures of patient perception to better characterize tourniquet effects in relation to patient-reported factors. Third, the methods used to assess intraoperative and postoperative blood loss may lack precision as a result of factors such as blood loss on drapes, plugged postoperative drainage systems, etc. Fourth, in the no-tourniquet group, a tourniquet was used for cementation in 64% of patients with a mean tourniquet time of 9 minutes. We are unsure if this limited time of tourniquet duration could have affected our study results, and conceivably this may have blunted the between-group differences. Lastly, this report does not provide data or guidance on the use of a tourniquet in same-day bilateral TKA. As a result of the increased intraoperative blood loss encountered without tourniquet use, it may be unwise to avoid tourniquet use in both limbs of a bilateral TKA because it may result in excessive intraoperative blood loss. The authors individualize tourniquet use in bilateral TKA. Typically the first TKA is performed without tourniquet use. If intraoperative blood loss is greater than 150 cc, a tourniquet is considered for the second TKA.
Increased intraoperative blood loss was observed when a tourniquet was not used, but no statistical differences were found in total (intraoperative + postoperative) blood loss between the tourniquet and no-tourniquet groups. Review of the literature shows the majority of studies confirm that intraoperative blood loss is greater if a tourniquet is not used [3, 11, 14, 17, 19, 22, 28, 29, 45, 49, 56, 58, 60, 65]. Reports analyzing total blood loss are conflicting with some demonstrating no differences with or without tourniquet use [1, 29, 49, 58], whereas others demonstrate reduced [3, 54] or increased [28, 58] total blood loss if a tourniquet is used. Some have evaluated the effect of tourniquet use on hidden blood loss (residual blood within the knee joint, extravasated blood into adjacent soft tissues [15], or blood loss resulting from hemolysis [46]) and observed it is higher if a tourniquet is used [28, 58]. It is theorized that tourniquet-induced ischemia results in sustained local reactive hyperemia lasting many hours after tourniquet deflation. This causes increased hemorrhage into adjacent traumatized tissue in the perioperative period [2, 25, 47]. Another proposed hypothesis is the increased fibrinolytic activity associated with tourniquet-induced ischemia causes bleeding in adjacent soft tissues postoperatively [25, 37]. Our results with this relatively small sample size do not support substantial additional hemorrhaging either with or without tourniquet use in that total blood loss and postoperative edema were not different between those patients whose procedures were performed under tourniquet control and those whose were not.
Numerous reports have found lower levels of pain when a tourniquet is not used [1, 11, 14, 27, 56]. Others have observed pain is greater with higher tourniquet inflation pressure [59, 63]. Although our examination of pain was purely descriptive (we were underpowered for a thorough statistical examination of group differences in all outcomes), the group means we observed suggest against a clinically meaningful effect of tourniquet use on postoperative pain levels. Determination of clinically relevant changes in pain is contextual and probably depends on the nature and risk of the procedure required to attain a given improvement [10, 18]. However, the numeric pain scale is typically associated with an MCID of approximately 2 points [50], and the mean differences observed in pain outcomes in our study were substantially smaller.
Small increments (2°-5º) of higher knee flexion mean values, likely of no clinical significance, were observed without tourniquet use at all testing intervals (preoperative until 3 months postoperatively). Most comparative reviews of tourniquet versus no-tourniquet use demonstrate superior knee flexion, especially in the first month after TKA, when a tourniquet was not used [11, 14, 60, 62, 65]. However, the improved knee flexion is not always maintained at longer-term followup evaluation [14, 60]. Group means for lower extremity edema also indicate that any differences would be unlikely to have clinical relevance. Other reports evaluating this outcome measure have similarly found no difference [56, 62] or less edema [11, 47] when a tourniquet is not used.
In this randomized trial, tourniquet use during TKA negatively impacted quadriceps strength during the first 3 postoperative months. The results of this evaluation have resulted in limited tourniquet use by the authors in primary TKA. Future studies may be warranted to examine the effects of tourniquet use on long-term strength and functional outcomes.
References
Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br. 1995;77:250–253.
Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M. Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res. 2000;371:169–177.
Alcelik I, Pollock RD, Sukeik M, Bettany-Saltikov J, Armstrong PM, Fismer P. A comparison of outcomes with and without a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. 2012;27:331–340.
Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010;40:559–567.
Behm D, Power K, Drinkwater E. Comparison of interpolation and central activation ratios as measures of muscle inactivation. Muscle Nerve. 2001;24:925–934.
Behm DG, St-Pierre DM, Perez D. Muscle inactivation: assessment of interpolated twitch technique. J Appl Physiol. 1996;81:2267–2273.
Berry DJ, Bozic KJ. Current practice patterns in primary hip and knee arthroplasty among members of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2010;25:2–4.
Bin Abd Razak HR, Tan HC. The use of pneumatic tourniquets is safe in Asians undergoing total knee arthroplasty without anticoagulation. Knee. 2014;21:176–179.
Butt U, Ahmad R, Aspros D, Bannister GC. Factors affecting wound ooze in total knee replacement. Ann R Coll Surg Engl. 2011;93:54–56.
Carragee EJ. The rise and fall of the ‘minimum clinically important difference.’ Spine J. 2010;10:283–284.
Chen S, Li J, Peng H, Zhou J, Fang H, Zheng H. The influence of a half-course tourniquet strategy on peri-operative blood loss and early functional recovery in primary total knee arthroplasty. Int Orthop. 2014;38:355–359.
Clarke MT, Longstaff L, Edwards D, Rushton N. Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg Br. 2001;83:40–44.
Din R, Geddes T. Skin protection beneath the tourniquet. A prospective randomized trial. ANZ J Surg. 2004;74:721–722.
Ejaz A, Laursen AC, Kappel A, Laursen MB, Jakobsen T, Rasmussen S, Nielsen PT. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85:422–426.
Erskine JG, Fraser C, Simpson R, Protheroe K, Walker ID. Blood loss with knee joint replacement. J R Coll Surg Edinb. 1981;26:295–297.
Feng L, Zhang XG, Yang QG, Wang G. [Effects of tourniquet on cardiac function in total knee arthroplasty with trans-esophageal echocardiography] [in Chinese]. Zhonghua Yi Xue Za Zhi. 2013;93:3755–3757.
Fukuda A, Hasegawa M, Kato K, Shi D, Sudo A, Uchida A. Effect of tourniquet application on deep vein thrombosis after total knee arthroplasty. Arch Orthop Trauma Surg. 2007;127:671–675.
Gatchel RJ, Mayer TG. Testing minimal clinically important difference: consensus or conundrum? Spine J. 2010;10:321–327.
Harvey EJ, Leclerc J, Brooks CE, Burke DL. Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplasty. 1997;12:291–296.
Hirota K, Hashimoto H, Tsubo T, Ishihara H, Matsuki A. Quantification and comparison of pulmonary emboli formation after pneumatic tourniquet release in patients undergoing reconstruction of anterior cruciate ligament and total knee arthroplasty. Anesth Analg. 2002;94:1633–1638, table of contents.
Horlocker TT, Hebl JR, Gali B, Jankowski CJ, Burkle CM, Berry DJ, Zepeda FA, Stevens SR, Schroeder DR. Anesthetic, patient, and surgical risk factors for neurologic complications after prolonged total tourniquet time during total knee arthroplasty. Anesth Analg. 2006;102:950–955.
Jarolem KL, Scott DF, Jaffe WL, Stein KS, Jaffe FF, Atik T. A comparison of blood loss and transfusion requirements in total knee arthroplasty with and without arterial tourniquet. Am J Orthop. 1995;24:906–909.
Kim JG, Lee SW, Ha JK, Choi HJ, Yang SJ, Lee MY. The effectiveness of minimally invasive total knee arthroplasty to preserve quadriceps strength: a randomized controlled trial. Knee. 2011;18:443–447.
Kittelson AJ, Stackhouse SK, Stevens-Lapsley JE. Neuromuscular electrical stimulation after total joint arthroplasty: a critical review of recent controlled studies. Eur J Phys Rehabil Med. 2013;49:909–920.
Klenerman L, Chakrabarti R, Mackie I, Brozovic M, Stirling Y. Changes in haemostatic system after application of a tourniquet. Lancet. 1977;1:970–972.
Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty. A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplasty. 1998;13:211–216.
Ledin H, Aspenberg P, Good L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012;83:499–503.
Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33:1263–1268.
Li X, Yin L, Chen ZY, Zhu L, Wang HL, Chen W, Yang G, Zhang YZ. The effect of tourniquet use in total knee arthroplasty: grading the evidence through an updated meta-analysis of randomized, controlled trials. Eur J Orthop Surg Traumatol. 2014;24:973–986.
Magee DJ, Zachazewski JE, Quillen WS. Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St Louis, MO, USA: Saunders Elsevier; 2007.
Meier W, Mizner RL, Marcus RL, Dibble LE, Peters C, Lastayo PC. Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther. 2008;38:246–256.
Mintken PE, Carpenter KJ, Eckhoff D, Kohrt WM, Stevens JE. Early neuromuscular electrical stimulation to optimize quadriceps muscle function following total knee arthroplasty: a case report. J Orthop Sports Phys Ther. 2007;37:364–371.
Mittal R, Ko V, Adie S, Naylor J, Dave J, Dave C, Harris IA, Hackett D, Ngo D, Dietsch S. Tourniquet application only during cement fixation in total knee arthroplasty: a double-blind, randomized controlled trial. ANZ J Surg. 2012;82:428–433.
Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35:424–436.
Mizner RL, Petterson SC, Stevens JE, Axe MJ, Snyder-Mackler L. Preoperative quadriceps strength predicts functional ability one year after total knee arthroplasty. J Rheumatol. 2005;32:1533–1539.
Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am. 2005;87:1047–1053.
Nakahara M, Sakahashi H. Effect of application of a tourniquet on bleeding factors in dogs. J Bone Joint Surg Am. 1967;49:1345–1351.
Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA, USA: FA Davis; 2009.
Olivecrona C, Blomfeldt R, Ponzer S, Stanford BR, Nilsson BY. Tourniquet cuff pressure and nerve injury in knee arthroplasty in a bloodless field: a neurophysiological study. Acta Orthop. 2013;84:159–164.
Olivecrona C, Lapidus LJ, Benson L, Blomfeldt R. Tourniquet time affects postoperative complications after knee arthroplasty. Int Orthop. 2013;37:827–832.
Olivecrona C, Ponzer S, Hamberg P, Blomfeldt R. Lower tourniquet cuff pressure reduces postoperative wound complications after total knee arthroplasty: a randomized controlled study of 164 patients. J Bone Joint Surg Am. 2012;94:2216–2221.
Parmet JL, Berman AT, Horrow JC, Harding S, Rosenberg H. Thromboembolism coincident with tourniquet deflation during total knee arthroplasty. Lancet. 1993;341:1057–1058.
Parmet JL, Horrow JC, Berman AT, Miller F, Pharo G, Collins L. The incidence of large venous emboli during total knee arthroplasty without pneumatic tourniquet use. Anesth Analg. 1998;87:439–444.
Parmet JL, Horrow JC, Singer R, Berman AT, Rosenberg H. Echogenic emboli upon tourniquet release during total knee arthroplasty: pulmonary hemodynamic changes and embolic composition. Anesth Analg. 1994;79:940–945.
Parvizi J, Diaz-Ledezma C. Total knee replacement with the use of a tourniquet: more pros than cons. Bone Joint J. 2013;95:133–134.
Pattison E, Protheroe K, Pringle RM, Kennedy AC, Dick WC. Reduction in haemoglobin after knee joint surgery. Ann Rheum Dis. 1973;32:582–584.
Silver R, de la Garza J, Rang M, Koreska J. Limb swelling after release of a tourniquet. Clin Orthop Relat Res. 1986;206:86–89.
Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg. 2001;9:253–257.
Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. 2010;17:141–147.
Stauffer ME, Taylor SD, Watson DJ, Peloso PM, Morrison A. Definition of nonresponse to analgesic treatment of arthritic pain: an analytical literature review of the smallest detectable difference, the minimal detectable change, and the minimal clinically important difference on the pain visual analog scale. Int J Inflamm. 2011;2011:231926.
Stevens-Lapsley JE, Bade MJ, Shulman BC, Kohrt WM, Dayton MR. Minimally invasive total knee arthroplasty improves early knee strength but not functional performance: a randomized controlled trial. J Arthroplasty. 2012;27:1812–1819 e1812.
Stevens-Lapsley JE, Balter JE, Kohrt WM, Eckhoff DG. Quadriceps and hamstrings muscle dysfunction after total knee arthroplasty. Clin Orthop Relat Res. 2010;468:2460–2468.
Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther. 2012;92:210–226.
Stroh DA, Johnson AJ, Mont MA, Bonutti PM. Excellent Clinical outcomes in total knee arthroplasty performed without a tourniquet. Surg Technol Int. 2011;XXI:189–193.
Sulek CA, Davies LK, Enneking FK, Gearen PA, Lobato EB. Cerebral microembolism diagnosed by transcranial Doppler during total knee arthroplasty: correlation with transesophageal echocardiography. Anesthesiology. 1999;91:672–676.
Tai TW, Chang CW, Lai KA, Lin CJ, Yang CY. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:2209–2215.
Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:1121–1130.
Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Canadian journal of surgery. Journal canadien de chirurgie. 2001;44:33–38.
Unver B, Karatosun V, Tuncali B. Effects of tourniquet pressure on rehabilitation outcomes in patients undergoing total knee arthroplasty. Orthop Nurs. 2013;32:217–222.
Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop. 2002;26:306–309.
Verbeke G, Molenberghs G. Linear Mixed Models in Practice: An SAS-oriented Approach. New York, NY, USA: Springer; 1997.
Wakankar HM, Nicholl JE, Koka R, D’Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 1999;81:30–33.
Worland RL, Arredondo J, Angles F, Lopez-Jimenez F, Jessup DE. Thigh pain following tourniquet application in simultaneous bilateral total knee replacement arthroplasty. J Arthroplasty. 1997;12:848–852.
Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech. 2008;23:320–328.
Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2014;9:13.
Acknowledgments
We acknowledge Kristin Schank PT, DPT, and Ward Carroll PT, DPT, for their assistance with inpatient testing; Kendall Slutzky for assistance with study coordination, including randomization of participants; Pamela Wolfe MS, for statistical analysis; and Joshua Winters PhD, for assistance with LabVIEW programming.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (DAD, CCY, TMM, RHK) has received funding from Porter Adventist Hospital, during the study period, in the amount of USD 10,000 to USD 100,000. One of the authors (DAD) has or may receive payments or benefits from DePuy (Warsaw, IN, USA) in the amount of USD more than USD 1,000,001 not related to this work. One of the authors certifies that he (RHK) has or may receive payments or benefits from Stryker (Kalamazoo, MI, USA) and Innomed (Savannah, GA, USA) in the amount of USD 100,001 to USD 1,000,001 not related to this work. One of the authors (TMM) has or may receive payments or benefits from Zimmer (Warsaw, IN, USA) in the amount of less than USD 10,000 not related to this work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
The surgeries for this study were performed at Porter Adventist Hospital, Denver, CO, USA, and the postoperative patient testing was performed at the University of Colorado Anschutz Medical Campus, Aurora, CO, USA.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Dennis, D.A., Kittelson, A.J., Yang, C.C. et al. Does Tourniquet Use in TKA Affect Recovery of Lower Extremity Strength and Function? A Randomized Trial. Clin Orthop Relat Res 474, 69–77 (2016). https://doi.org/10.1007/s11999-015-4393-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4393-8